- fruit and diabetes. Blueberries good, cantaloupe bad.
- R most popular language for “analytics/data mining/data science work” among survey respondents. I wish I could describe the respondents, but I can only say they are people who might call what they do “data mining” or “data science”. In addition, the use of R is growing. Most psychology departments teach SPSS or Matlab.
- Thomas Frank criticizes universities, undergraduate education in particular. “An educational publisher wrote to me [asking] to reprint an essay of mine [that is freely available]. . . . The low, low price that students were to pay for this textbook: $75.95.”
Category: blood sugar
Assorted Links
- electric field perception by humans
- Umami plate
- Jana Beck confirms that a low-carb diet improves her blood sugar levels
- “Goldman Sachs got the FBI to do its bidding” (Felix Salmon)
- Whey protein reduces after-meal blood sugar rise. Whey protein is in cheese, for example.
- Several unpleasant aspects of surgery prep unhelpful
Thanks to Alex Chernavsky.
Organic Pollutants Associated With Diabetes
Everyone knows that diabetes is associated with obesity, probably because obesity causes diabetes. However, thin people also become diabetic. A clue to why is provided by the correlation between diabetes and what are called “persistent organic pollutants” (POPs). POPs are man-made organic compounds, usually pesticides, such as polychlorinated dibenzo-p-dioxins and polychlorinated dibenzofurans.
A 2006 study using NHANES (National Health and Nutrition Examination Survey 1999–2002) data found very strong associations between levels of these chemicals and diabetes. For example, a risk ratio of 30. These associations persisted even when the data was stratified in all sorts of ways. The scariest result came from people who had BMI < 25. Looking only at such people, those above the 90th percentile for amount of POPs had 16 times the risk of diabetes as those below the 25th percentile. Here is something associated with thin people getting diabetes.
Does the association exist because POPs cause diabetes? You might argue that POP exposure is correlated with poverty (poor people are more exposed), poor people exercise less than rich people, and lack of exercise causes diabetes. However, Agent Orange exposure among soldiers is associated with diabetes. That is unlikely to be due to confounding with poverty or lack of exercise.
Everyone has these chemicals in their body, but almost no one knows how much. I don’t know if I’m in the 10th percentile or the 90th percentile. If I’m in the 90th percentile, what can I do about it? A good place for self-measurement and tracking.
Assorted Links
- Walking after a meal improves blood sugar
- A look at QSers. “S ome of the most societally redefining concepts now emerge from edge-thinkers, who are increasingly visible, organized, and effective, in part due to the Web. Even so, whenever I spoke to them or read their blogs, at some point I always wondered, why?”
- Steve McIntyre vindicated. RealClimate says: “That is the most disquieting legacy of Steve McIntyre and ClimateAudit [McIntyre’s blog]. The real Yamal deception is their attempt to damage public confidence in science by making speculative and scandalous claims about the actions and motivations of scientists while cloaking them in a pretense of advancing scientific knowledge.” A comment on ClimateAudit: “It’s quite obvious that in 2009 and again in 2011, you shamelessly plagiarised Briffa 2013.”
Thanks to Jazi Zilber and Phil Alexander.
Does Alternate-Day Fasting Lower HbA1c?
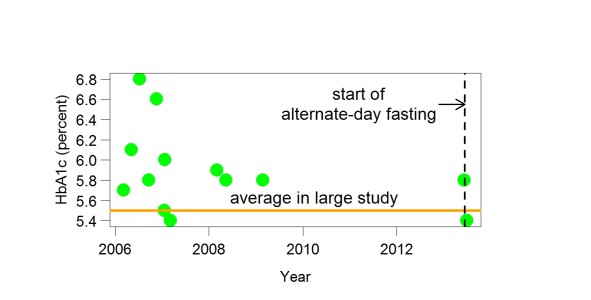
This graph shows my HbA1c values in recent years. After a lot of variation, they settled down to 5.8, which was the measurement a month ago. 5.8 isn’t terrible — below 6.0 is sometimes called “okay”) — but there is room for improvement. In a large 2010 study, average HbA1c was 5.5. The study suggested that a HbA1c of about 5.0 was ideal.
Three weeks ago I started alternate-day fasting (= eating much less than usual every other day) for entirely different reasons. Although people sometimes find alternate-day fasting unpleasant (they get too hungry on the fast days), I haven’t noticed this. I blogged recently that within days of starting, my fasting blood sugar levels greatly improved. Yesterday I got my HbA1c measured again. It was 5.4 — much better. This supports the idea that alternate-day fasting is helping a lot. HbA1c measures glucose in the blood over 8-12 weeks so there could easily be more improvement.
“Whether intermittent fasting can be used as a tool to prevent diabetes in those individuals at high risk or to prevent progression in those recently diagnosed with Type 2 diabetes remains a tantalizing notion,” said an author of a recent paper on the subject. My experience suggests that you can easily find out for yourself if intermittent fasting will help. It took only a week to be sure that my fasting blood sugar had improved and only three weeks to have a good idea that my HbA1c has improved. My improvement was almost as fast and clear as what happens when people with a vitamin deficiency are given the vitamin they need.
There are countless ways of doing alternate-day fasting (or, more generally, intermittent fasting). A clinical trial usually tests just one way, which you may not want to copy exactly. My results suggest that blood sugar measurements provide an easy way to tell if your particular version of intermittent fasting is helping.
Alternate-Day Fasting Improved My Fasting Blood Sugar
A few days ago, I gave a talk at a Quantified Self Meetup in San Francisco titled “Why is my blood sugar high?” (PowerPoint here and here). My main point was that alternate-day fasting (eating much less than usual every other day) quickly brought my fasting blood sugar level from the mid-90s to the low 80s, which is where I wanted it. I was unsure how to do this and had tried several things that hadn’t worked.
Not in the talk is an explanation of my results in terms of setpoint (blood sugar setpoint, not body fat setpoint). Your body tries to maintain a certain blood sugar level — that’s obvious. Not obvious at all is what controls the setpoint. This question is usually ignored — for example, in Wikipedia’s blood sugar regulation entry. Maybe Type 2 diabetes occurs because the blood sugar setpoint is too high. If we can find out what environmental events control the setpoint, we will be in a much better position to prevent and reverse Type 2 diabetes (as with obesity).
A few years ago, I discovered that walking an hour per day improved my fasting blood sugar. Does walking lower the setpoint? I didn’t ask this question, a curious omission from the author of The Shangri-La Diet. If walking lowered the setpoint, walking every other day might have the same effect as walking every day.
I was pushed toward this line of thought because alternate-day fasting seems to lower the blood-sugar setpoint. After I started alternate-day fasting, it took about three days for my fasting blood sugar to reach a new lower level. After that, it was low every day, not just after fast days. My experience suggests that the blood-sugar setpoint depends on what your blood sugar is. When your blood sugar is high, the setpoint becomes higher; when your blood sugar is low, the setpoint becomes lower. Tim Lundeen had told me something similar to this.
If you tried to lower your fasting blood sugar and succeeded, I hope you will say in the comments how you did this. I tried three things that didn’t work: darker bedroom, Vitamin B supplement, and cinnamon. Eating low carb raises fasting blood sugar, according to Paul Jaminet.
Assorted Links
- The Data Vigilante
- Unnecessary wisdom tooth extractions
- How American medicine is destroying itself (their title, not mine). “Look at the “breakthroughs” that have been predicted for such scientific sure things as stem-cell technology and medical genetics—but have yet to be realized. . . Our [= American medicine’s] main achievements today consist of devising ways to marginally extend the lives of the very sick.”
- New kind of light bulb, matches sunlight much better. I believe building lighting will eventually match sunlight during the day and not match it (removing the blue light that controls circadian clocks, such as the clock that puts you to sleep) after sundown. Improving sleep and health.
- Exposure to pesticides used to purify water correlated with allergies. Water with fewer microbes may be more dangerous than water with more microbes.
- Diabetes: the epidemic. Unlike other major causes of death — heart disease, stroke, and cancer — diabetes is increasing quickly.
Thanks to Dave Lull and Alex Chernavsky.